Our Services
We provide all modalities of medical diagnostic ultrasound:
- Echocardiogram
- Carotid Ultrasoundv
- Lower Extremity Arterial Doppler w/ ABI’s
- Upper Extremity Arterial Doppler
- Lower Extremity Venous Doppler
- Upper Extremity Venous Doppler
- Abdominal Ultrasound
- Female Pelvic Ultrasound (transabdominal & transvaginal)
- Male Pelvic Ultrasound (Prostate)
- Retroperitoneal (Renal) Ultrasound
- Bladder Ultrasound
- Renal Artery Doppler
- Thyroid Ultrasound
- Abdominal Aorta Ultrasound
- Testicular Ultrasound
- Hemodialysis Access Graft
- Cardiovascular Screenings
- Pseudoaneurysm Compression
ECHOCARDIOGRAM
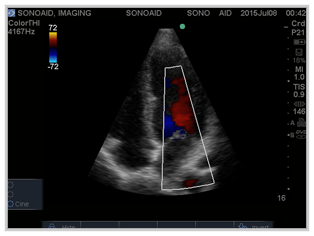 An echocardiogram (often called “echo”) is a test in which ultrasound is used to examine the heart. In addition to providing single-dimension images, known as M-mode that allows accurate measurement of the heart chambers, the echocardiogram also offers far more sophisticated and advanced (2-D) two-dimensional imaging and is capable of displaying a cross-sectional real time slice of the beating heart, including the chambers, valves and the major blood vessels that exit from the left and right ventricle. This procedure is combined with Doppler ultrasound and color Doppler to evaluate blood flow across the heart’s valves. The Doppler exam reflects sound waves off the moving red blood cells within the heart chambers to reveal the speed and direction of blood flow within the heart. This is helpful in evaluating function of the valves. Color Flow Mapping shows the speed and direction of blood flow via a color graphic. Color Flow Mapping allows the Cardiologist to “map” abnormalities in blood flowing through the heart and great vessels.
An echocardiogram (often called “echo”) is a test in which ultrasound is used to examine the heart. In addition to providing single-dimension images, known as M-mode that allows accurate measurement of the heart chambers, the echocardiogram also offers far more sophisticated and advanced (2-D) two-dimensional imaging and is capable of displaying a cross-sectional real time slice of the beating heart, including the chambers, valves and the major blood vessels that exit from the left and right ventricle. This procedure is combined with Doppler ultrasound and color Doppler to evaluate blood flow across the heart’s valves. The Doppler exam reflects sound waves off the moving red blood cells within the heart chambers to reveal the speed and direction of blood flow within the heart. This is helpful in evaluating function of the valves. Color Flow Mapping shows the speed and direction of blood flow via a color graphic. Color Flow Mapping allows the Cardiologist to “map” abnormalities in blood flowing through the heart and great vessels. Indications:
- Symptoms potentially due to suspected cardiac etiology, including but not limited to dyspnea, shortness of breath, palpitations, lightheadedness, syncope, TIA, cerebrovascular events
- Prior testing that is concerning for heart disease (chest x-ray, baseline stress echo, ECG, serum BNP elevation)
- Known or suspected congenital heart disease, arrhythmias, aortic disease
- Pulmonary hypertension
- Hypotension or hemodynamic instability
- Heart murmur
- Valve function evaluation, stenosis, regurgitation, infective endocarditis, mitral valve prolapse
- Evaluation of intra- and extra-cardiac structures and chambers
- LV function evaluation
- Acute myocardial infarction
- Coronary insufficiency
- Cardio-toxic agent monitoring
- Pericardial disease detection
- Hypertension
- Chest pain
- Murmur
- Syncope
- Arrhythmia
- Coronary artery disease
- Valvular heart disease
- Endocarditis
- Pulmonary disease
- Cardiac masses
- Evaluation of ventricular function
- Stroke
- Peripheral emboli involving major arteries
- Family history of genetic cardiac disorder
The exam takes approximately 45 minutes.
There are no special preparations or instructions for this exam.
Vascular Ultrasound
Carotid Duplex Imaging
Lower Extremity Arterial Duplex Imaging
Upper Extremity Arterial Duplex Imaging
Lower Extremity Venous Duplex Imaging
Upper Extremity Venous Duplex Imaging
Carotid Duplex Imaging
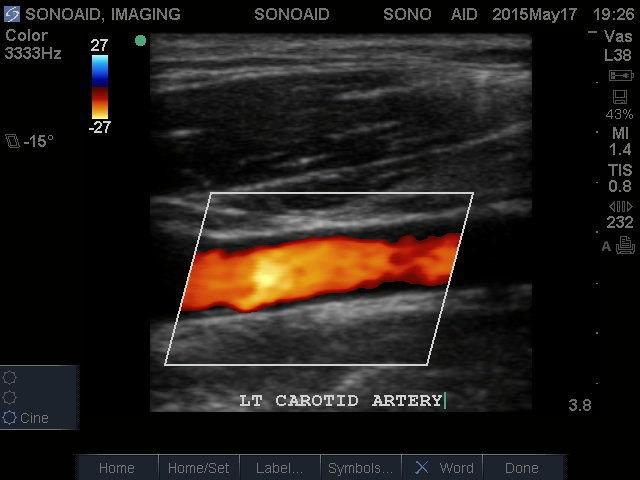 A carotid artery duplex scan is a safe non-invasive (the skin is not pierced) diagnostic assessment of the blood flow through the vessels that supply the neck and brain. The term “duplex” refers to the fact that two modes of ultrasound are used – Doppler and B-mode. The B-mode is an image of the carotid artery being studied; the Doppler evaluates the velocity and direction of blood flow in the vessel.
A carotid artery duplex scan is a safe non-invasive (the skin is not pierced) diagnostic assessment of the blood flow through the vessels that supply the neck and brain. The term “duplex” refers to the fact that two modes of ultrasound are used – Doppler and B-mode. The B-mode is an image of the carotid artery being studied; the Doppler evaluates the velocity and direction of blood flow in the vessel.
The duplex scan has become the definitive test in the diagnosis of carotid arterial disease. This test affords superior visualization of plaque thickness and accumulation within the carotid artery, while other types of blood flow problems are assessed with this procedure.
Carotid ultrasound is also used as a preventive screening test in people who have previously diagnosed medical conditions that increase their risk of stroke, including high blood pressure and diabetes. People with these conditions may benefit from having their carotid arteries checked regularly even if they show no signs of plaque buildup.
Indications:
- Abnormal sound observed in carotid artery
- Blood clots/slowed blood flow in the carotid artery
- Had a stroke or ministroke recently
- Split/Weakness in the tissues of the carotid artery wall
- Episodic dizziness
- Cerebral embolization
- Cervical or carotid bruit
- Memory Loss
- Cluster type headache
- Loss of balance
- Vertigo
- Loss of vision/field cut
- Aphasia/dysphasia
- Increased vessel wall rigidity found during palpati
- Motor or sensory deficit
- Diplopia
- Syncope
- Unilateral paresthesias
- Drop attacks
- Amaurosis Fugax (transient monocular blindness)
- Fluctuating confusion
- Numbness/tingling
The exam takes approximately 45 minutes.
There are no special preparations or instructions for this exam.
Arterial Duplex – Upper and Lower Extremities
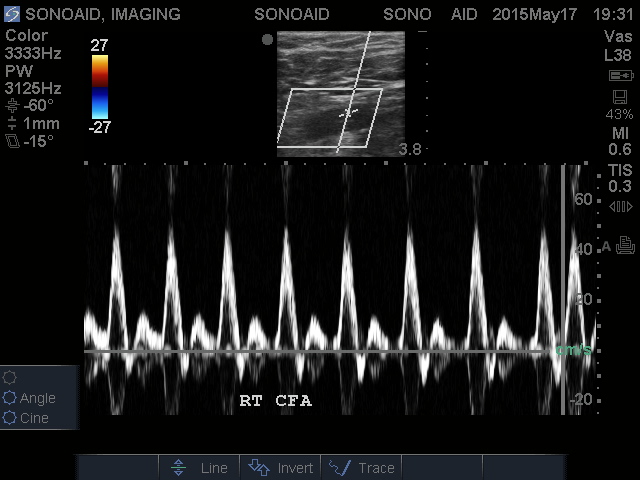 Duplex ultrasonography of the upper and lower extremity arteries is performed to provide an overview of the location, extent and severity of vascular disease. The lower extremity Doppler evaluation is performed from the iliacs through the tibial vessels and extended into the foot, while the upper extremity variant can be performed from the subclavian artery to the wrist.
Duplex ultrasonography of the upper and lower extremity arteries is performed to provide an overview of the location, extent and severity of vascular disease. The lower extremity Doppler evaluation is performed from the iliacs through the tibial vessels and extended into the foot, while the upper extremity variant can be performed from the subclavian artery to the wrist.
Sites of suspected stenosis are evaluated with Doppler measurements proximal to, within, and distal to maximum stenosis.
Duplex imaging determines the plaque length in arterial segments and patency of distal vessels. Arterial imaging will also help determine if claudication is associated with arterial disease or musculoskeletal or neuropathic reasons. A controlled trial of the effectiveness of imaging procedures suggested that the results of Duplex ultrasound were comparable to those of contrast angiography, in terms of surgical planning and outcome.
Indications:
- Evaluation or follow-up of patients with claudication, ischemic rest pain, and/or arterial ulceration
- Assessment of patients with documented arterial disease
- Pre-procedure assessment for planning of intervention
- Follow-up to determine technical adequacy of surgical intervention, i.e., post angioplasty and/or stent placement
- Follow-up of bypass grafts to detect intrinsic stenosis or progression of disease, which may threaten graft patency
- Evaluation of aneurysm, pseudoaneurysm and arterial-venous fistula
- Evaluation of arterial trauma
- Absent or diminished distal or pedal pulse
- Diabetes with peripheral circulatory disorder
- Skin or nail infections
- Skin color changes or ulcerations
- Distal extremity hair loss
- Gangrene
- Extreme weakness or fatigue
- Vasomotor instability
- Numbness
- PAD
The ankle brachial index (ABI) is a noninvasive test used to determine a patient’s risk for peripheral artery disease, a condition that involves a narrowing of the arteries in the leg and can lead to a heart attack or stroke. It is performed by placing blood pressure cuffs on your arms and ankle as you lie on your back. A gel will be applied on the crease of your elbow and a Doppler pen (a type of ultrasound transducer) will be placed in the same area to measure the blood pressure. The blood pressure will be then taken on your legs by placing the Doppler pen on the artery above your ankle. An ABI (Ankle Brachial Index) number is then calculated by the systolic blood pressure of your leg divided by the blood pressure in your arms.
The ABI results will determine whether you have Peripheral Arterial Disease or not based on your Index. The ABI range that is generally considered normal is 0.95 to 1.20.
Indications:
- Peripheral artery disease
- Deep vein thrombosis
- Arterial trauma
- Aneurysm, pseudoaneurysm and arterial-venous fistula
- Carotid occlusive disease
- Abdominal aneurysm
- Assessment of patients with documented arterial disease
- Renal vascular insufficiency
- Evaluation or follow-up of patients with claudication, ischemic rest pain, and/or arterial ulceration
- Diabetes with peripheral circulatory disorder
- Pre-procedure assessment for planning of intervention
- Follow-up to determine technical adequacy of surgical intervention, i.e., post angioplasty and/or stent placement
- Follow-up of bypass grafts to detect intrinsic stenosis or progression of disease, which may threaten graft patency
- Absent or diminished distal or pedal pulse
- Skin or nail infections
- Skin color changes or ulcerations
- Distal extremity hair loss
- Gangrene
- Extreme weakness or fatigue
- Vasomotor instability
- Numbness
Venous Duplex – Upper and Lower Extremities
 Venous duplex imaging is used to evaluate blood clots, venous insufficiency, varicose veins, incompetence or tumor/masses obstructed veins. Acute and chronic thrombosis can be differentiated. In addition, this procedure may be used to detect superficial phlebitis and obstruction.
Venous duplex imaging is used to evaluate blood clots, venous insufficiency, varicose veins, incompetence or tumor/masses obstructed veins. Acute and chronic thrombosis can be differentiated. In addition, this procedure may be used to detect superficial phlebitis and obstruction.
Patients at an increased risk for lower extremity peripheral venous disease may include those with previous deep vein and/or superficial vein thrombosis (DVT/SVT), lower extremity trauma, immobilization of extremity, recent major surgery, prolonged bed rest, history of cancer, family history of DVT, pregnancy, congestive heart failure (CHF) or other similar cardiac problems.
Upper extremity DVT most often affects patients with previous upper extremity vein thrombosis or trauma, recent or past surgery on the affected extremity (recent or prior dialysis access graft surgery, dialysis catheter, central venous line or chemotherapy access port insertions), and history of cancer.
Upper Extremity Venous Indications:
- Deep vein thrombosis
- Arm swelling
- Vein mapping prior to surgery
- Arm pain
Lower Extremity Venous Indications:
- Leg pain
- Leg swelling
- Skin discoloration of the leg
- Varicose veins
- Deep vein thrombosis
- Leg sores
- Vein mapping prior to surgery
- Phlebitis
- Edema
Abdominal Aortic Duplex
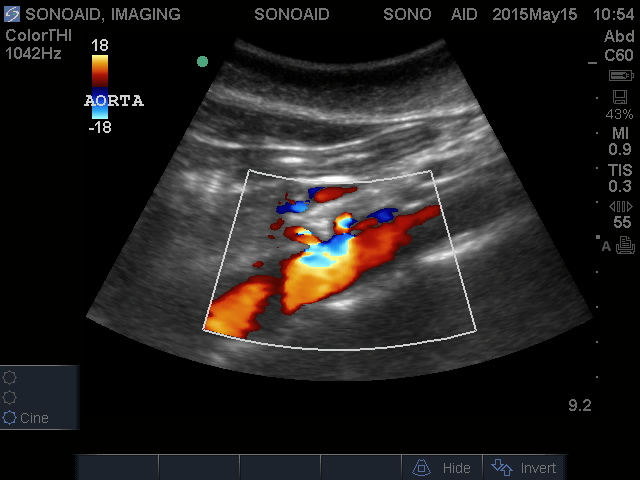 This is a non-invasive exam. The patient will be lying on their back during the exam. A water based gel will be applied on the abdomen. A transducer (probe) will scan this area to view the abdominal aorta. The procedure takes 20 minutes.
This is a non-invasive exam. The patient will be lying on their back during the exam. A water based gel will be applied on the abdomen. A transducer (probe) will scan this area to view the abdominal aorta. The procedure takes 20 minutes.The exam will determine if the diameter of the aorta is in the normal range or not. If the diameter of the aorta is greater than 3cm, this is called an abdominal aortic aneurysm (AAA).
Abdominal Aortic Aneurysm (AAA)
Proteins in the wall of the aorta, called elastin and collagen provide strength and flexibility to this large artery. This is similar to muscles and tendons providing strength to the arms and legs. Aneurysms are caused by a progressive breakdown of these proteins that lead to a weakness of the wall of the aorta that can steadily expand like a balloon. These proteins, collagen and elastin, may gradually deteriorate with age. Inflammation, that is associated with atherosclerosis (hardening of the arteries), helps to accelerate this degenerative process even in younger people. When the diameter of the aorta is greater than 3 cm it is considered an aortic aneurysm.
The Society for Vascular Surgery and the Society for Vascular Medicine and Biology recommends the following courses of action after screening:
- No further testing if aortic diameter is less than 3.0 cm;
- Yearly ultrasonographic screening if aortic diameter is between 3.0 to 4.0 cm;
- Ultrasonography every 6 months if aortic diameter is between 4.0 to 4.5 cm;
- Referral to a vascular specialist if aortic diameter is greater than 4.5 cm.
Benefits of early detection
When aortic aneurysms are diagnosed early, treatment is safe and effective and the aneurysm is curable. Aneurysms are often detected while performing tests for entirely different reasons. Most patients have no symptoms, so if you are at risk, it is important to discuss AAA with your doctor. Early diagnosis will identify if you require surgery and can thereby prevent rupture or leakage of the aneurysm. Early intervention reduces AAA specific mortality.
Risk Factors
- Age over 60 years.
- Family history of AAA.
- Tobacc
- use.
- History of heart disease or peripheral arterial disease.
- High blood pressure (hypertension).
Abdominal Ultrasound
 An Abdominal Ultrasound is performed to visually evaluate abdominal organs, including the liver, gallbladder, pancreas, bile ducts, abdominal aorta and spleen, to help detect a wide range of conditions and also assess blood flow to these organs.
An Abdominal Ultrasound is performed to visually evaluate abdominal organs, including the liver, gallbladder, pancreas, bile ducts, abdominal aorta and spleen, to help detect a wide range of conditions and also assess blood flow to these organs.Ultrasound can detect tumors, cysts, abscesses, obstructions, fluid collection, clots and infection in the abdomen Negative findings are important for exclusion of diseases and, therefore, for reassurance of the patient. Abdominal Ultrasound substantially reduced the number of intended referrals to a medical specialist, and more patients could be reassured by their General Practioner.
There is no discomfort, risk or radiation exposure with ultrasound. There are some conditions that may interfere with the results of the abdominal ultrasound exam. The most common are severe obesity, intestinal gas and barium in the intestines from a GI series that was performed prior to the ultrasound exam.
Indications:
- Abdominal pain is the most common indication for an abdominal ultrasound.
- Abnormal liver function
- Enlarged abdominal organ
- Stones in the gallbladder or kidney
- Abnormal laboratory results suggestive for abdominal pathology
- Search for metastatic disease
- Palpable abnormalities
PELVIC ULTRASOUND
 A pelvic ultrasound is performed to visualize the organs within the pelvis, including the bladder, ovaries, prostate and other related structures in order to detect and evaluate conditions such as cancer, fibroids, ovarian cysts, kidney stones and urinary tract infections. Doppler ultrasound technology may be used to view blood flow through the pelvis for a more accurate diagnosis. Male and female ultrasound exams may be performed using different techniques.
A pelvic ultrasound is performed to visualize the organs within the pelvis, including the bladder, ovaries, prostate and other related structures in order to detect and evaluate conditions such as cancer, fibroids, ovarian cysts, kidney stones and urinary tract infections. Doppler ultrasound technology may be used to view blood flow through the pelvis for a more accurate diagnosis. Male and female ultrasound exams may be performed using different techniques.Female Pelvic Ultrasound
Transvaginal and transabdominal
These type of exams are a noninvasive (the skin is not pierced) procedure used to assess organs and structures within the female pelvis. A pelvic / transvaginal ultrasound allows quick visualization of the female pelvic organs and structures including the uterus, cervix vagina, fallopian tubes, and ovaries.
Indications:
- Pelvic Pain which is a common complaint patients present due to entities such as ovarian cysts, tubo-ovarian abscesses, and uterine fibroids.
- Pelvic mass
- Pelvic Infection particularly tubo-ovarian abscesses which are difficult to diagnose at physical examination.
- Pelvic Trauma to evaluate for free fluid or clotted blood, which can be present in the pouch of Douglas (cul-de-sac).
- Abnormal Uterine Bleeding in the premenopausal patient as well as the postpartum and post abortion patient.
- Bladder Stone Identification
- Blockages to Blood Flow (such as clots).
- Narrowing of Vessels (which may be caused by plaque)
Male pelvic ultrasound is used to evaluate:
- Prostate
- Bladder
- Seminal vesicles
Renal Ultrasound
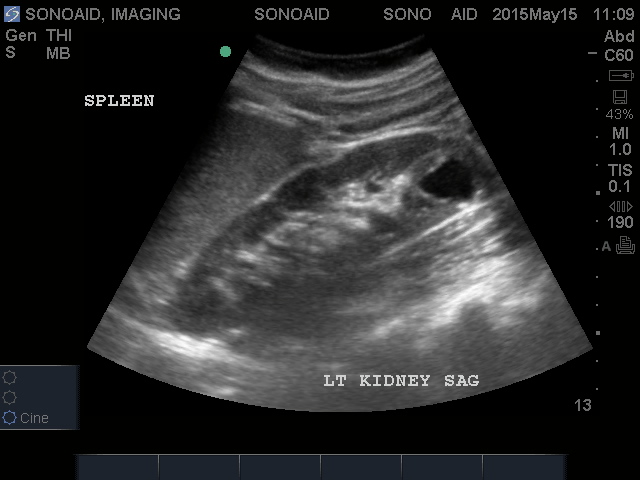
Indications:
- Flank pain, hematuria or abnormal renal function
- Assessment of renal and perirenal mass found on physical examination or other imaging study
- Assessment of dilated upper urinary tract
- Postoperative evaluation after renal and ureteral surgery
- To assess the dynamics of the upper tract effects of voiding
- Evaluation for and monitoring of urolithiasis
- Intra-operative renal parenchymal and vascular imaging for ablation or resection of masses
- Evaluation of hematuria in patients who are not candidates for IVP, CT or MRI.
- Percutaneous access to renal collecting system
- To guide transcutaneous renal biopsies, cyst aspiration or ablation of masses
- Evaluation of postoperative renal transplant patients
- Interior Vena Cava, detection of invasion by tumor & filter localization
- To preclude obstruction in symptomatic patients
- Changes in the bladder wall
- Changes in kidney size or structure
- Kidney stone, cyst, mass, or other obstruction in the kidney
- Stones in the urinary tract
- Changes in the ureters
Renal Artery Duplex
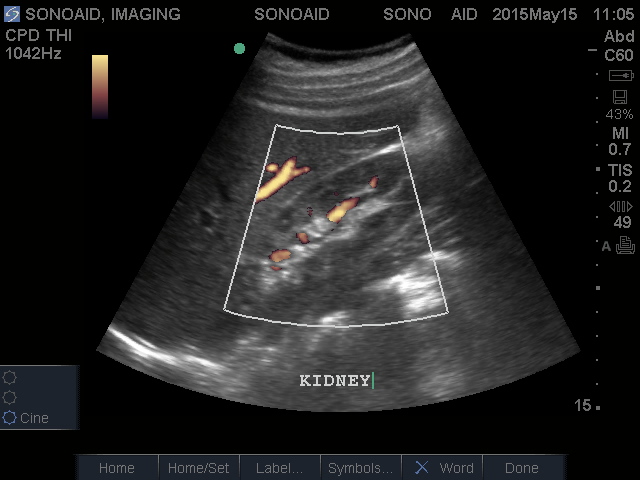 Renal artery duplex imaging evaluates blood flow velocities and patterns in the aorta and renal arteries. According to the American College of Radiology, “Ultrasound using grayscale imaging, Doppler spectral analysis, and color Doppler imaging is a proven and useful procedure for evaluating the renovascular system.” Many patients with hypertension are referred for a renal artery duplex because of their increased risk of renal artery stenosis. Some cases of renovascular hypertension actually develop as a result of an obstruction in the renal arteries. These cases of hypertension can usually be effectively treated by treating the obstruction. Flow patterns within the kidneys can provide information about damage to the kidneys and extent of renal artery disease from chronic poor blood flow. Color Doppler can show renal artery perfusion and venous return. It may also be used to determine renal transplant rejection.
Renal artery duplex imaging evaluates blood flow velocities and patterns in the aorta and renal arteries. According to the American College of Radiology, “Ultrasound using grayscale imaging, Doppler spectral analysis, and color Doppler imaging is a proven and useful procedure for evaluating the renovascular system.” Many patients with hypertension are referred for a renal artery duplex because of their increased risk of renal artery stenosis. Some cases of renovascular hypertension actually develop as a result of an obstruction in the renal arteries. These cases of hypertension can usually be effectively treated by treating the obstruction. Flow patterns within the kidneys can provide information about damage to the kidneys and extent of renal artery disease from chronic poor blood flow. Color Doppler can show renal artery perfusion and venous return. It may also be used to determine renal transplant rejection.Indications:
- Evaluation of patients with hypertension
- Evaluation of the native renal arteries and kidneys for evidence of renal artery disease or renal
- Parenchymal disease
- Presence of epigastric or flank bruit in a hypertensive patient
- Screening for renal artery stenosis prior to medical management with ACE inhibitors
- Presence of elevated creatinine or BUN
- Monitoring of known renal artery stenosis
- Suspected renal vein occlusion
- Renal artery embolus
- Suspected renal artery aneurysm
- Suspected arteriovenous fistula
- Presence of a thrill or bruit following renal biopsy
- Evaluation of renal transplant dysfunction
- Presence of bruit over renal transplant
Testicular Ultrasound

Indications:
- Monitor recurring testicular cancer
- Fluid within the scrotum (hydrocele) or epididymis (spermatocele)
- Blood in the scrotum (hematocele)
- Injury evaluation
- Mass in the testicles
Thyroid Ultrasound
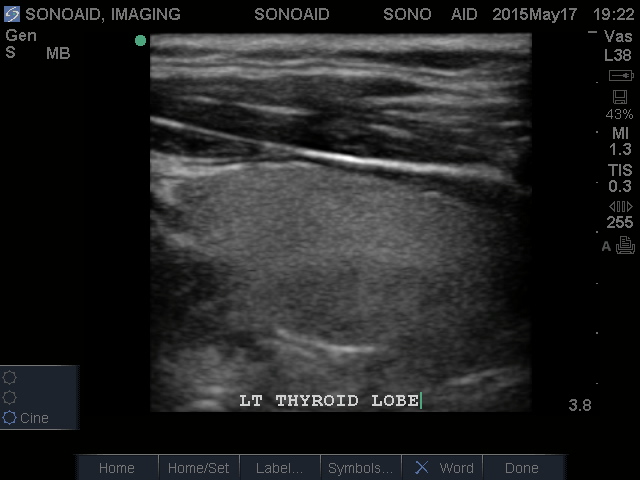
Indications:
- Evaluation of the location and characteristics of palpable neck masses
- Abnormal Thyroid function test
- Thyroiditis
- Abnormalities detected by other imaging examinations or laboratory studies, including areas of abnormal uptake seen on radioisotope thyroid examinations.
- Evaluation of the presence, size, and location of the thyroid gland.
- High-risk patients for occult thyroid malignancy.
- Follow-up of thyroid nodules, when indicated.
- Recurrent disease or regional nodal metastases in patients with proven or suspected thyroid carcinoma.
Musculoskeletal Ultrasound
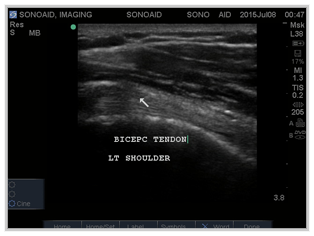
Indications:
- Tendon: Tendons in many parts of the body are readily visible with ultrasound, in particular the shoulder, ankle and Achilles tendon.
- Bursae: A swollen bursa can be detected with ultrasound, most commonly used around the shoulder and knee joints.
- Ligaments: Some ligaments can be demonstrated with ultrasound.
- Foreign Bodies: Not all foreign bodies will be visible using x-rays. Most will be identified with ultrasound. The location and damage to any surrounding structures is readily seen.
24 to 48 hour turnaround time for finalized reports.
Same day reports for STAT exams.
At SonoAid Imaging we offer a variety of services and tests including mobile ultrasound.
In order to better understand our services please call us at (818) 241-2514 to set up an appointment or send us an e-mail by clicking here.




